Alcohol Focus Scotland call on the Scottish Government through the briefing document below, with a call for ‘Urgent Action on Alcohol Deaths’.
Call for Urgent Action to Reduce Alcohol Deaths
Key Points
•Over 70 stakeholders, including local Alcohol and Drug Partnerships, charities and medical Royal Colleges, are calling for urgent action to address the highest level of alcohol deaths in 15 years.
•Alcohol harm is a public health emergency, as recognised by the Scottish Government in 2021.
•Alcohol harm affects families, communities, our NHS and wider public services. The cost to Scottish society is an estimated £10 billion each year.
•80% of adults drink and 20% of adults regularly exceed the low-risk guidelinesi, increasing their risk of experiencing long-term and life limiting health conditions such as cancer, heart conditions and stroke.
•Scottish Government action is not proportionate to the scale of the problem we face.
•Deaths are expected to rise further due to the impact of the pandemic on drinking patterns and on services.
•The number of people in treatment dropped by 40% in the ten years to 2021/22 and services report people presenting later and with more complex needs.
•Audit Scotland has highlighted the lack of investment and focus on alcohol services.
•Scottish Government has accepted Audit Scotland’s recommendation that they must, by mid-2025 “work with key stakeholders to identify and agree actions to increase focus and funding for tackling alcohol-related harm.”
•As key stakeholders, we call on the Scottish Government to take the following urgent actions to reduce deaths:
Increase early diagnosis for liver disease
Establish Alcohol Care Teams (ACTs) in acute hospital
Improve access to alcohol detoxification services
Increase funding for tackling alcohol harm
We also call on the Scottish Government to develop and implement a comprehensive and integrated alcohol strategy which takes a preventative approach to reducing alcohol harm
Alcohol Deaths and Harm: An Ongoing Crisis
In 2021 the Scottish Government rightly recognised alcohol harm as a public emergency,alongside drug deaths. Since then, alcohol-specific deaths have risen to a 15 year high.
Alcohol specific deaths in Scotland 1994-2023, National Records of Scotland
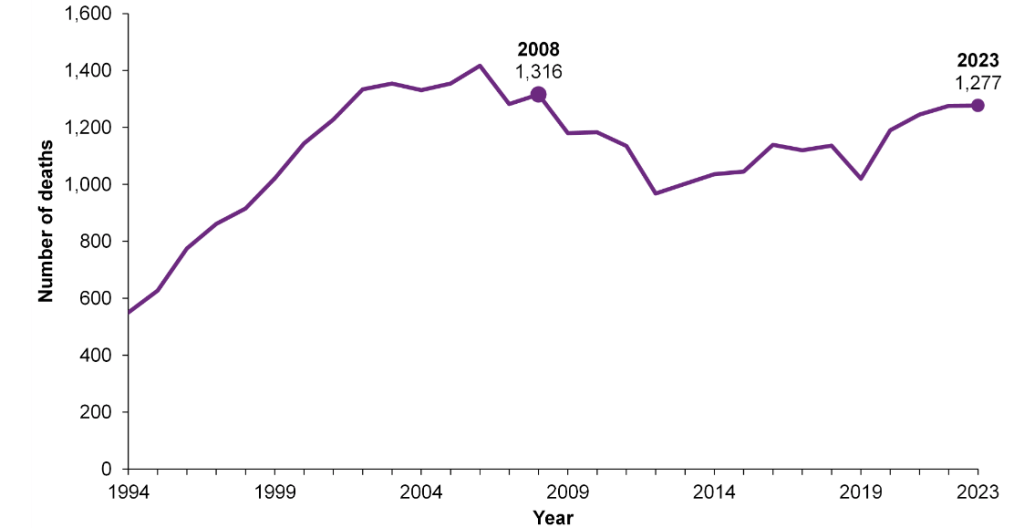
The latest figures show 1,277 people lost their lives to alcohol-specific causes in 2023.iii Yet even these figures only show the tip of the iceberg; Public Health Scotland estimate that the total number of deaths caused by alcohol is likely to be more than double.iv The alcohol-specific statistics only capture deaths from conditions that are caused by alcohol alone, such as alcohol-related liver disease and alcohol dependence syndrome. In fact, most deaths due to alcohol are from wider alcohol-related causes, such as cancers, heart conditions, stroke, and accidental injuries. Each is a life cut tragically short and leaves behind family and friends suffering their loss.
Unfortunately, the COVID-19 pandemic and restrictions have exacerbated Scotland’s alcohol problem, with increased harmful drinking and reduced access to services driving increased harm. If these changes in consumption persist into the long term, it is estimated that this will lead to around 7,500 more deaths and 70,000 more hospitalisations by 2040, costing £82 million in hospital costs alone. Anecdotally, services report higher demand and greater complexity in cases, with people presenting in poorer health.
Recent figures reveal that access to alcohol treatment is at its lowest in a decade, with a 40% decline in the number of people starting specialist alcohol treatment from 2013/14 to 2021/22. Although the Scottish Government has tasked Public Health Scotland with investigating this decline, it is clear that there is both a failure to prevent harm and a gap in treating it.
Our alcohol problem is disproportionately felt by people living in Scotland’s most deprived communities, where individuals are over four times more likely to die due to alcohol and six times more likely to be hospitalised compared to those living in the wealthiest areas. When harm increases, it affects these communities most severely.
While deaths are the most extreme form of alcohol harm, they are likely to be accompanied by increases in other harms which can impact those experiencing alcohol problems as well those around them. These impacts can themselves be life-changing and include alcohol-related diseases, accidents, violence, unemployment, family and relationship breakdown, domestic abuse, child neglect and Fetal Alcohol Spectrum Disorder. This is compromising people’s right to health, which the Scottish Government has a legal duty to respect, protect and fulfil. None of this is inevitable. By taking action now we can save and improve thousands of lives.
Scottish Government’s Response is Not Proportionate
The Scottish Government has committed to, taken, or initiated, a number of actions to tackle the alcohol harm emergency,ix including:
•the continuation and uprating of Minimum Unit Pricing;
•a PHS review of Alcohol Brief Interventions (ABIs);
•a PHS review of evidence on protecting children and young people from alcohol marketing;
•the incorporation of UK-wide clinical guidelines for alcohol treatment services into a National Service Specification for alcohol and drugs services;
•the National Mission’s increase in residential rehabilitation capacity resulting in increased rehab capacity for people with alcohol problems; and
•work with SHAAP on raising awareness of the link between alcohol and cancer amongst health professionals and with AFS to provide guidance on conducting alcohol death reviews.
These actions are welcome and much needed, but it is clear that they are not sufficient to reverse the increasing tide of harm. Indeed, many of these actions have been planned or underway for some time, while others represent a delay. Work on alcohol marketing is actually a step back from the Scottish Government’s previous commitment to bring forward a consultation on specific proposals by the end of 2024 and Audit Scotland has highlighted that progress in this area has been slow. Nor do these actions represent a coordinated and cohesive approach to addressing the near-record levels of alcohol deaths and harm in Scotland.
This is in sharp contrast to the Scottish Government’s response to the public health emergency of drugs deaths, which has involved a far more strategic and coordinated approach, including:
•establishment of a Drug Deaths Taskforce (2019-22);
•appointment of a dedicated Minister for Drug Policy in 2020 (remit extended to cover alcohol in 2023);
•establishment of a National Mission in 2021, supported by an additional £250m funding over 5 years;
•publication of a National Mission plan 2022-26;
•analysis of local Alcohol and Drugs Partnerships annual reports to evidence progress on the National Mission;
•the introduction of new standards for Medication Assisted Treatment;
•an evaluation of the National Mission by Public Health Scotland.
Audit Scotland highlighted this significant gap in effort and funding in their recent report into alcohol and drug services, noting that while the National Mission on Drugs has provided a focus on drug-related harm, “there have been no equivalent developments specifically focusing on reducing alcohol harm.” The Auditor General, himself, stated: “The creation of the National Mission has in part been at the expense of focus on alcohol deaths and alcohol services.”
Audit Scotland’s first recommendation is that by mid-2025 the Scottish Government must “work with key stakeholders to identify and agree actions to increase focus and funding for tackling alcohol-related harm.” The Director-General for Health and Social Care and Chief Executive of NHS Scotland has confirmed that the Scottish Government accepts this recommendation. We agree with Audit Scotland’s recommendation and we call on the Scottish Government to:
•take urgent action to identify and support those at risk from alcohol deaths
•provide clear leadership on alcohol by developing a comprehensive and preventative strategy to reduce alcohol harm.
Four Urgent Actions Required to Reduce Alcohol Deaths
To address the rising alcohol-related deaths, we propose four urgent actions that will enable people with serious or potentially life-threatening alcohol problems to be identified sooner and supported more effectively. This will reduce their risk of experiencing more serious harm and improve their health and wellbeing.
1.Increase Early Diagnosis for Liver Disease
Liver disease is one of the leading causes of premature deaths in Scotland, above breast cancer and suicide,xiii with cases of chronic liver disease expected to increase by 54% from 2019 to 2044.xiv Over 70% of liver disease deaths are attributable to alcoholxv and over 60% of alcohol-specific deaths are due to liver disease.iii It is known as the ‘silent killer’ as three-quarters of cirrhosis patients are diagnosed in emergency departments, when it is too late for effective treatment or intervention.xvi If detected earlier, alcohol-related liver disease can be reversed.
Expanding liver testing in community alcohol settings will enable those at high risk to be identified sooner and provided with care and support to address their liver problem and their alcohol use. Non-invasive liver tests like FibroScan have been found to improve abstinence amongst people who are using alcohol servicesxvii xviii and are recommended for use amongst those who consume alcohol at harmful levels by the National Institute for Health and Care Excellence (NICE) in England and Wales.
In North-East Glasgow, FibroScans have been used since 2019 to identify liver damage among people attending alcohol services. Around 400 scans a year are conducted, identifying around a quarter of patients as having significant liver fibrosis and 1 in 10 as having possible cirrhosis. Insights from this approach should guide the deployment of these technologies in community alcohol settings across Scotland. Investment in devices and healthcare staffing and training will be vital to ensure early detection resources reach high-need areas.
2.Establish Alcohol Care Teams (ACTs) in acute hospitals
Admission to hospital, whether due to an injury or an illness, is the ideal opportunity to identify if a person has an alcohol use disorder, including dependence. If an alcohol problem is identified, intervention and access to more comprehensive alcohol treatment can be provided, including a pathway to community services upon discharge from the hospital. Some models already exist in England and there are examples of elements of Alcohol Care Teams being taken forward in some hospitals in Scotland, but this is inconsistent.
Establishing nurse-led Alcohol Care Teams (ACTs) in all acute hospitals would ensure that patients with severe alcohol problems or dependence are identified and are provided with safe, specialised, multidisciplinary support to address their alcohol problem. xxi By operating within the hospital setting, ACTs can provide both immediate care and establish clear referral pathways to appropriate treatment services, and it is a way of preventing repeat hospital admissions.
3.Improve Access to Alcohol Detoxification Services
For people with severe alcohol problems, detoxification can be a vital first step in beginning their recovery. However, unlike withdrawal from other drugs, suddenly reducing or stopping drinking can cause serious, potentially life-threatening, issues. There is emerging evidence that services to support people during their detox are not operating optimally, in part due to changes implemented during the pandemic.
Improving access to effective detoxification services is essential to ensuring that heavy and dependent drinkers can access help to reduce or stop drinking safely, avoiding acute withdrawal. A range of detox support options is needed: within hospitals, in residential rehabilitation services and in the community. All should operate on the basis of supporting successful detox and ensuring people are referred to on-going support and treatment. This will reduce people’s risk of experiencing a ‘revolving door’ where they relapse and require further detox. It will also increase their chances of beginning their journey to sustainable recovery.
4.Increase Funding for Tackling Alcohol Harm
Earlier identification and treatment will make more efficient use of resources over time. However, as Audit Scotland has highlighted, alcohol services have been under-funded for some time and additional investment is urgently required.
The Scottish Government has made an additional £1.5 million available for alcohol and drugs in 2025/26. However, even if all of this is directed towards alcohol – and there is no indication that it will be – this level of resource will have limited impact on the existing treatment gap.
What is needed is more substantial, on-going investment. This could be generated through re-introducing a levy on alcohol retailers, using a simple, tried and tested approach using existing order making powers.xxii The Fraser of Allander Institute have estimated that such a levy could generate around £60m per year, with 86% of the revenue coming from large supermarket chains.
Call to Develop and Implement a New Alcohol Strategy
While the above actions are urgent, we believe that to fundamentally address the negative impact of alcohol on people, families, communities as well as our NHS, social and criminal justice services, the Scottish Government must take a more sustained and systemic approach. Seven years on from the launch of Alcohol Framework (2018) and Rights, Respect, and Recovery (2018), we are calling for the development and delivery of a new alcohol strategy.
The strategy should develop a comprehensive and integrated preventative system, drawing on Public Health Scotland’s Public Health Approach to Prevention. This recognises that action across all three types of prevention – primary, secondary and tertiary – is central to addressing poor outcomes and reducing inequalities.
The new alcohol strategy should continue to prioritise the World Health Organization’s ‘best buy’ policies of increasing the price, reducing the availability, and restricting the marketing of alcohol. Such universal approaches that target the whole population are most effective at preventing health harms and reducing health inequalities.
The strategy should include the following preventative actions:
•Introduce automatic uprating of the minimum unit price (MUP) for alcohol to optimise the effectiveness of the policy in saving and improving lives.
•Reform the system for licensing off-trade and online sales to firstly cap and then reduce off-trade availability of alcohol.
•Restrict alcohol marketing, including advertising outdoors, in public spaces and sport and event sponsorships, as well as displays in shops.
•Mandate the provision of health-related information, including health warnings, on alcohol products
In order to inform the development of strategic priorities for future recovery-oriented treatment, care and support provision, a National Needs Assessment for Alcohol is required. No such assessment has been undertaken since 2014 and the scale and shape of people’s needs and the barriers they face in accessing support have changed significantly, not least due to the impacts of the pandemic.
The new strategy must also be firmly grounded in a human rights-based approach, embedding human rights – such as the highest attainable standard of health and an adequate standard of living – across prevention, treatment and support. This includes protecting individuals from harmful alcohol marketing, prioritising community well-being in policy interventions, and ensuring equitable access to services. The Charter of Rights for People Affected by Substance Use, developed by the National Collaborative, provides a framework to uphold dignity and respect for those in need of support, based on national and international law. The Scottish Government must now turn these rights into action, using the new strategy as a means to ensure they are not just guiding principles but a reality for those impacted by alcohol harm.
Signatories
1.Alcohol Focus Scotland
2.Alcohol and Drugs Support South West Scotland
3.Alcohol Health Alliance UK
4.Abbeycare
5.Association of Anaesthetists
6.Blue Triangle
7.British Heart Foundation Scotland
8.British Liver Trust
9.British Society of Gastroenterology
10.Carers Trust Scotland
11.Children First
12.Children in Scotland
13.Faculty of Public Health
14.Families Campaign for Change
15.FASS (Family Addiction Support Service)
16.Glasgow Council on Alcohol
17.GPs at the Deep End
18.Health and Social Care Alliance Scotland (The ALLIANCE)
19.Institute of Alcohol Studies
20.LGBT Health and Wellbeing
21.Liber8
22.Mungo Foundation
23.National Addiction Centre, Institute of Psychiatry, Psychology & Neuroscience (IoPPN), King’s College London
24.NCD Alliance Scotland
25.Queen’s Nursing Institute Scotland
26.Recovery Scotland
27.Royal College of Emergency Medicine
28.Royal College of General Practitioners
29.Royal College of Nursing
30.Royal College of Physicians of Edinburgh
31.Royal College of Physicians and Surgeons of Glasgow
32.Royal College of Psychiatrists
33.Royal Society for Public Health
34.Scottish Alcohol Counselling Consortium (SACC)
35.Scottish Cancer Foundation
36.Scottish Drugs Forum
37.Scottish Families Affected by Alcohol and Drugs (SFAD)
38.Scottish Health Action on Alcohol Problems (SHAAP)
39.Scottish Recovery Consortium
40.Simon Community
41.Stroke Association
42.The Canmore Trust
43.The European Alcohol Policy Alliance (Eurocare)
44.The International Youth Health Organization
45.The Salvation Army
46.The Salvation Army Centre for Addiction Services and Research
47.Together (Scottish Alliance for Children’s Rights)
48.Turning Point Scotland
49.UCL Tobacco & Alcohol Research Group
50.Wellbeing Economy Alliance Scotland (WEAll Scotland)
51.With You
52.World Cancer Research Fund International
53.Aberdeenshire ADP
54.City of Edinburgh ADP
55.Dumfries & Galloway ADP
56.East Ayrshire ADP
57.East Dunbartonshire ADP
58.East Renfrewshire ADP
59.Falkirk ADP
60.Glasgow City ADP
61.Highland ADP
62.Inverclyde ADP
63.Mid and East Lothian ADP
64.Moray ADP
65.North Ayrshire ADP
66.North Lanarkshire ADP
67.Orkney Islands ADP
68.Outer Hebrides ADP
69.Renfrewshire ADP
70.Scottish Borders ADP
71.South Lanarkshire ADP
72.West Dunbartonshire ADP

